Why the Warburg effect is still correct?
The Warburg effect, proposed by Otto Warburg in the 1920s, describes the observation that cancer cells often exhibit a distinct metabolic phenotype characterized by increased glucose uptake and fermentation of glucose to lactate even in the presence of oxygen (aerobic glycolysis).
 Warburg hypothesis/effect
Warburg hypothesis/effect
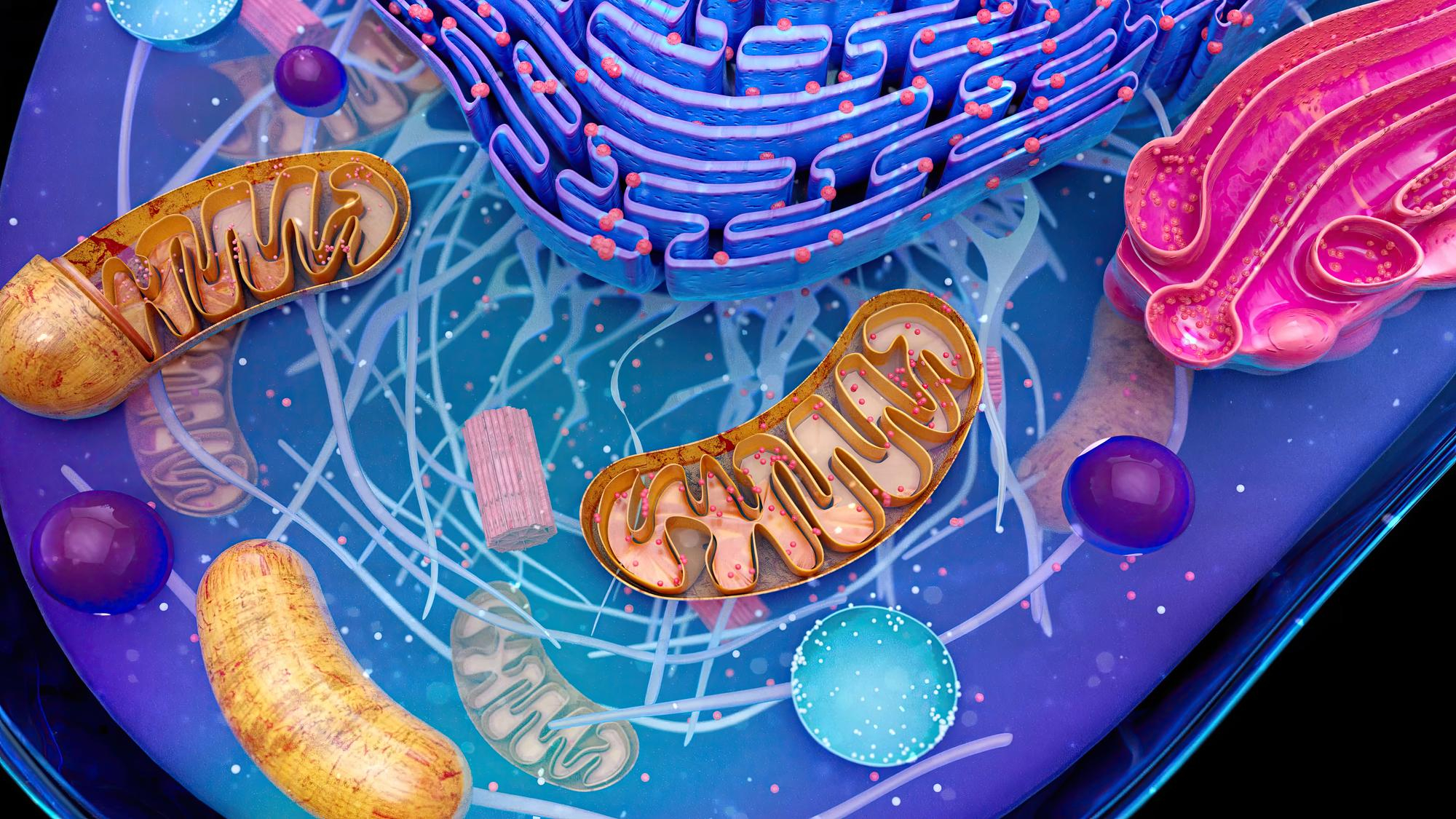
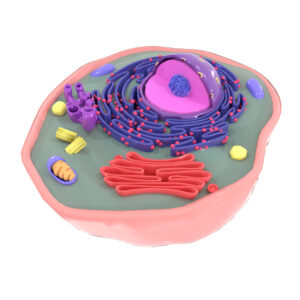
Cancer cells mainly produce energy by an increased rate of glycolysis (200 times more as compared to normal tissues of origin) followed by fermentation of lactate in the cytosol of the cell, even if oxygen is plentiful. This is to fulfill their bioenergetic and biosynthetic demands to support rapid proliferation. This observation in oncology is called the ‘Warburg effect’. In normal cells however the rate of aerobic glycolysis is lower, and is followed by oxidative phosphorylation in the mitochondria, where pyruvate is oxidated. It was postulated by Otto Warburg that this metabolic change is the fundamental cause of cancer [9], a claim now known as the Warburg hypothesis. However, it was then discovered that mutations in oncogenes and tumour suppressor genes are responsible for malignant transformation. Instead of a cause, the Warburg effect is considered to be more of a result of these genetic mutations.
Despite being proposed nearly a century ago, the Warburg effect remains relevant and widely studied for several reasons:
- Ubiquitous Phenomenon: The Warburg effect is observed in a wide variety of cancer types and has been replicated in numerous studies using modern techniques. This metabolic alteration appears to be a common feature of cancer cells regardless of their tissue of origin.
- Energetic Demands: Cancer cells have high energy demands to support rapid proliferation and survival under often hypoxic conditions within tumors. Aerobic glycolysis, despite being less efficient in terms of ATP production per molecule of glucose, allows cancer cells to quickly generate energy and metabolic intermediates needed for biomass synthesis.
- Regulatory Mechanisms: Molecular and genetic studies have identified various mechanisms that regulate the Warburg effect in cancer cells. These include alterations in oncogenes (e.g., MYC, RAS) and tumor suppressors (e.g., TP53), as well as signaling pathways (e.g., PI3K-AKT-mTOR pathway) that influence glucose metabolism.
- Clinical Implications: The Warburg effect has clinical implications for cancer diagnosis and treatment. It is exploited in imaging techniques such as positron emission tomography (PET) scans using fluorodeoxyglucose (FDG), which detects increased glucose uptake in tumors. Targeting metabolic vulnerabilities associated with the Warburg effect is also an active area of cancer therapy research.
- Evolutionary Advantage: Cancer cells may benefit from the Warburg effect beyond just energy production. It can provide substrates for biosynthetic pathways necessary for cell proliferation and survival, such as nucleotide and lipid synthesis.
- Tumor Microenvironment: The microenvironment within tumors, including hypoxia and nutrient deprivation, can drive the Warburg effect. Understanding how cancer cells adapt metabolically to their surroundings is crucial for developing effective therapies.
- Therapeutic Targets: Exploiting metabolic vulnerabilities associated with the Warburg effect has led to the development of novel therapeutic strategies, such as inhibitors of glycolysis or other metabolic pathways, to selectively target cancer cells while sparing normal cells.
In summary, the Warburg effect remains relevant and correct in the context of cancer biology due to its widespread occurrence across cancer types, underlying molecular mechanisms, clinical implications, and potential as a therapeutic target. While our understanding of cancer metabolism continues to evolve, the fundamental observations made by Otto Warburg have provided a solid foundation for ongoing research into metabolic alterations in cancer cells.