Overview
What is pancreatic cancer?
Pancreatic cancer occurs when cells in your pancreas mutate (change) and multiply out of control, forming a tumor. Your pancreas is a gland in your abdomen (belly), between your spine and stomach. It makes hormones that control blood-sugar levels and enzymes that aid in digestion.
Signs and symptoms
Unfortunately, there aren’t any early signs of pancreatic cancer. Symptoms typically emerge once the tumor starts impacting other organs in your digestive system.
Pancreatic cancer symptoms may include:
- Jaundice (yellowing of your skin).
- Dark urine (pee).
- Light-colored stool (poop).
- Upper abdominal pain.
- Middle back pain.
- Fatigue.
- Itchy skin.
- Nausea and vomiting.
- Gas or bloating.
- Lack of appetite.
- Blood clots.
- Weight loss.
- New-onset diabetes.


Pancreatic cancer and mitochondrial function
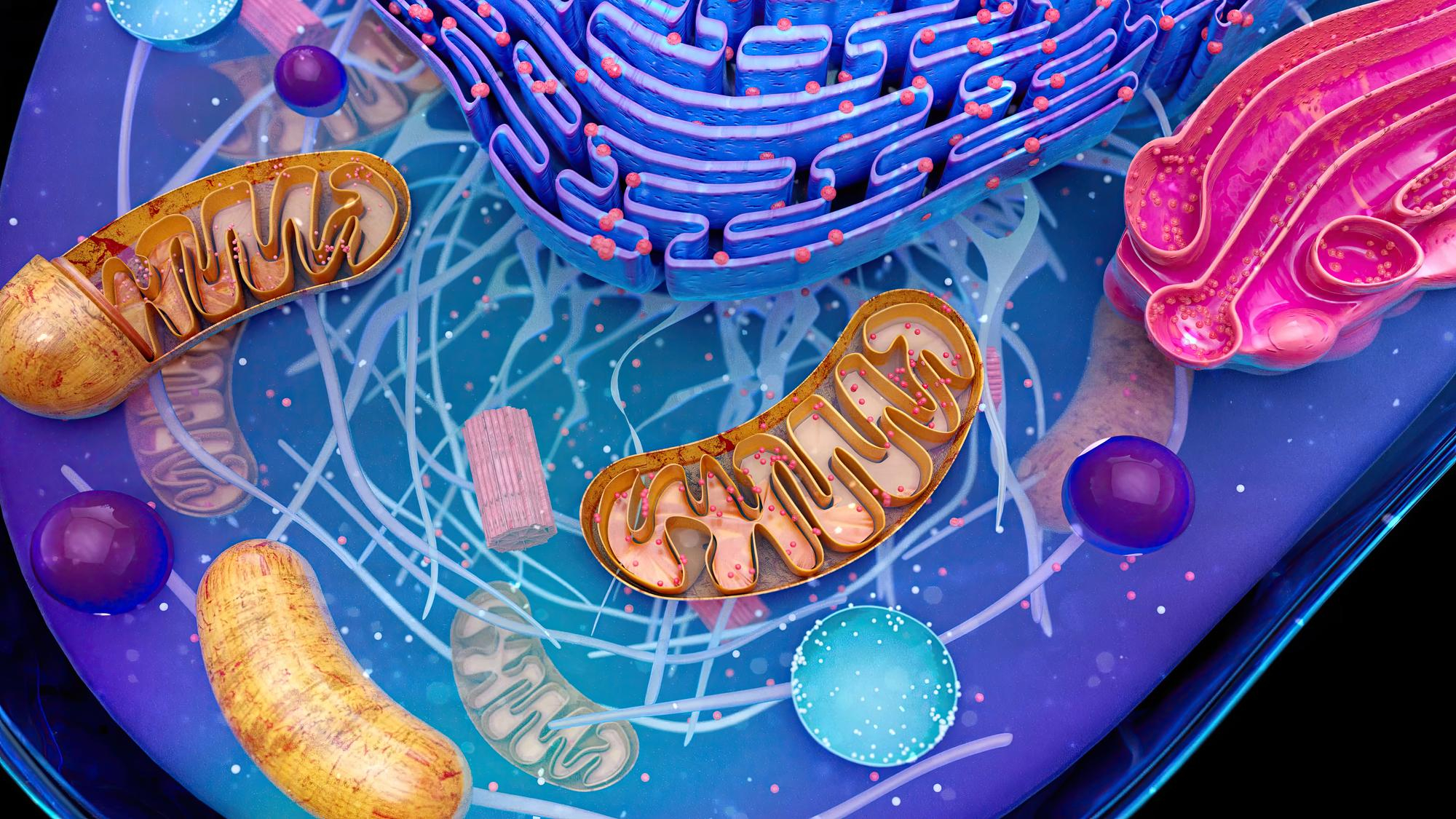
The role of mitochondria in tumor progression manifests primarily in three areas: metabolic reprogramming, anti-apoptotic mechanisms, and immune escape, all of which are crucial for cancer progression and resistance to therapy
In the field of pancreatic cancer research, multiomics analyses have played a pivotal role in elucidating the impact of mitochondrial gene defects. Alterations in the mitochondrial genome (mtDNA), such as mutations or deletions, have been associated with increased chemoresistance and metastatic capabilities in various cancer types. Moreover, recent studies have highlighted the potential of microRNAs that regulate mtDNA-encoded mitochondrial proteins (mitomiRs) and nuclear-encoded mitochondrial proteins as valuable biomarkers for cancer diagnosis and prognosis. For example, in the diagnosis of pancreatic cancer, several miRNAs (pancreatic intraepithelial neoplasia) have already been identified by researchers in the PanIN (pancreatic intraepithelial neoplasia) staging of pancreatic cancer, allowing us to study them as potential biomarkers.
Pancreatic ductal adenocarcinoma is a highly lethal neoplasia, and the currently used therapeutic approaches are not effective in a wide range of patients. Indeed, PDAC is one of the oncologic diseases with the lowest 5-years survival rate. As reported above, its aggressiveness is due to the absence of consistent early diagnostic markers and efficacious therapies. Thus, there is a need to deeply study the biological features of pancreatic cancer and cancer stem cells to improve patient survival. Due to the importance of regulating cellular functions, especially metabolic energy, mitochondria may represent key targets to be hit. However, as deeply described in this review, these organelles are plastic, and their fusion and division process represents an aspect that could discriminate among normal, tumoral, and cancer stem cells. In fact, modification of the fusion/fission equilibrium within the cells affects cellular function, both in physiological and pathological conditions.


Overview
What is pancreatic cancer?
Pancreatic cancer occurs when cells in your pancreas mutate (change) and multiply out of control, forming a tumor. Your pancreas is a gland in your abdomen (belly), between your spine and stomach. It makes hormones that control blood-sugar levels and enzymes that aid in digestion.

Signs and symptoms
Unfortunately, there aren’t any early signs of pancreatic cancer. Symptoms typically emerge once the tumor starts impacting other organs in your digestive system.
Pancreatic cancer symptoms may include:
- Jaundice (yellowing of your skin).
- Dark urine (pee).
- Light-colored stool (poop).
- Upper abdominal pain.
- Middle back pain.
- Fatigue.
- Itchy skin.
- Nausea and vomiting.
- Gas or bloating.
- Lack of appetite.
- Blood clots.
- Weight loss.
- New-onset diabetes.

Pancreatic cancer and mitochondrial function
The role of mitochondria in tumor progression manifests primarily in three areas: metabolic reprogramming, anti-apoptotic mechanisms, and immune escape, all of which are crucial for cancer progression and resistance to therapy
In the field of pancreatic cancer research, multiomics analyses have played a pivotal role in elucidating the impact of mitochondrial gene defects. Alterations in the mitochondrial genome (mtDNA), such as mutations or deletions, have been associated with increased chemoresistance and metastatic capabilities in various cancer types. Moreover, recent studies have highlighted the potential of microRNAs that regulate mtDNA-encoded mitochondrial proteins (mitomiRs) and nuclear-encoded mitochondrial proteins as valuable biomarkers for cancer diagnosis and prognosis. For example, in the diagnosis of pancreatic cancer, several miRNAs (pancreatic intraepithelial neoplasia) have already been identified by researchers in the PanIN (pancreatic intraepithelial neoplasia) staging of pancreatic cancer, allowing us to study them as potential biomarkers.

Pancreatic ductal adenocarcinoma is a highly lethal neoplasia, and the currently used therapeutic approaches are not effective in a wide range of patients. Indeed, PDAC is one of the oncologic diseases with the lowest 5-years survival rate. As reported above, its aggressiveness is due to the absence of consistent early diagnostic markers and efficacious therapies. Thus, there is a need to deeply study the biological features of pancreatic cancer and cancer stem cells to improve patient survival. Due to the importance of regulating cellular functions, especially metabolic energy, mitochondria may represent key targets to be hit. However, as deeply described in this review, these organelles are plastic, and their fusion and division process represents an aspect that could discriminate among normal, tumoral, and cancer stem cells. In fact, modification of the fusion/fission equilibrium within the cells affects cellular function, both in physiological and pathological conditions.