Overview
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumours. If left unchecked, the tumours can spread throughout the body and become fatal. Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. Cancer cells can spread into nearby breast tissue (invasion). This creates tumours that cause lumps or thickening.
Signs and symptoms
Most people will not experience any symptoms when the cancer is still early hence the importance of early detection. Breast cancer can have combinations of symptoms, especially when it is more advanced. Symptoms of breast cancer can include:
- a breast lump or thickening, often without pain
- change in size, shape or appearance of the breast
- dimpling, redness, pitting or other changes in the skin
- change in nipple appearance or the skin surrounding the nipple (areola)
- abnormal or bloody fluid from the nipple.
People with an abnormal breast lump should seek medical care, even if the lump does not hurt.


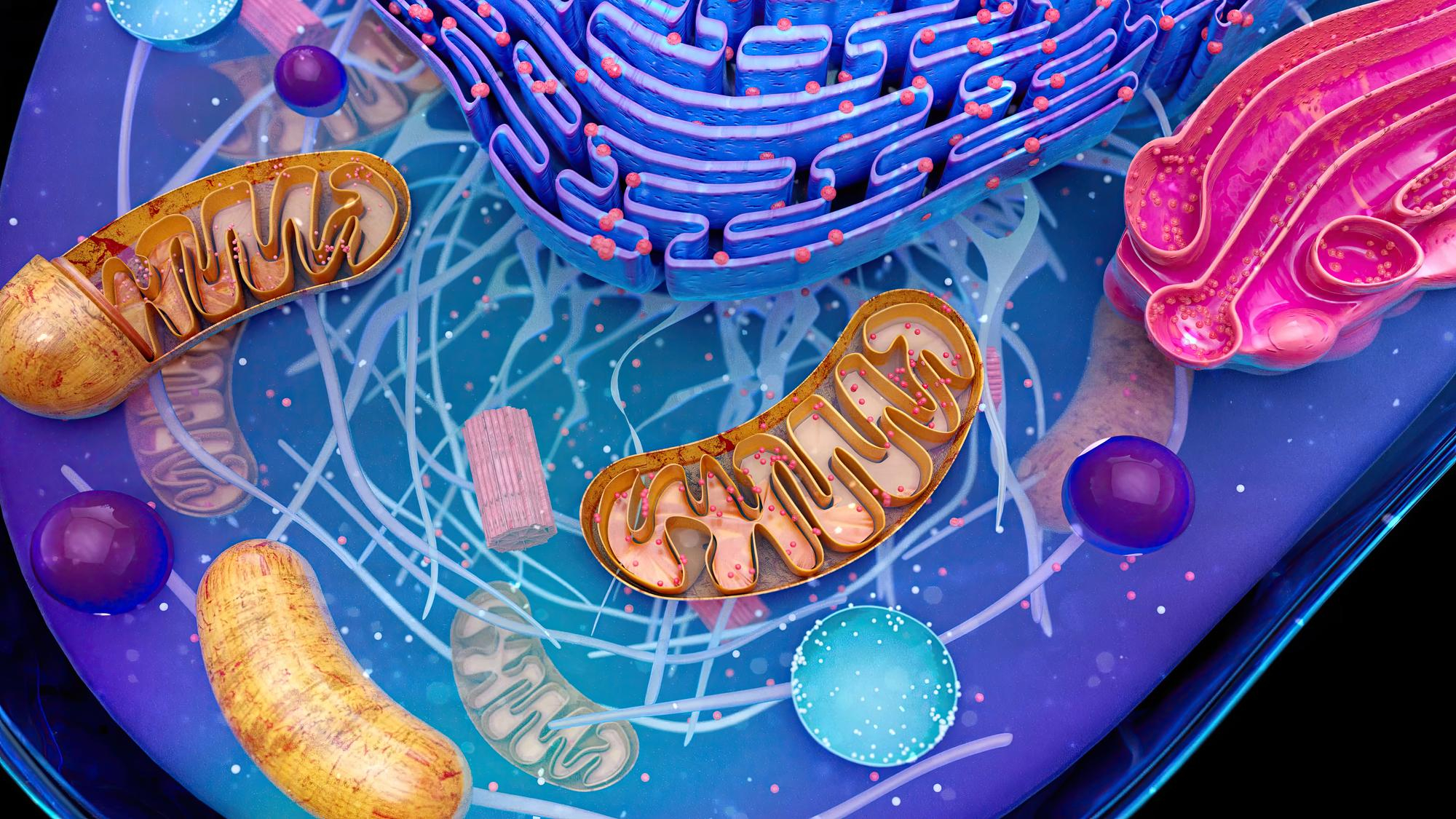
As a major energy source for cells, mitochondria are involved in cell growth and proliferation, as well as migration, cell fate decisions, and many other aspects of cellular function. Once thought to be irreparably defective, mitochondrial function in cancer cells has found renewed interest, from suggested potential clinical biomarkers to mitochondria-targeting therapies.
The flow of mitochondria from surrounding cells in breast cancer
Broadly, this phenomenon involves the movement of either whole mitochondria or mtDNA between cells and can be stimulated via several methods, including cell fusion, extracellular vesicles, tunneling nanotubes (TNTs), and through gap junctions (which may be close-ended TNTs). The free release of mitochondria has also been observed in culture medium and human plasma, but it is debated whether they are functional. Cell fusion is the process by which two independent cells partially or fully merge to create a singular cell (permanently or temporarily), thus mixing mitochondria. In vitro, normal (primary cells), neoplastic (MCF10A), and cancerous (MCF7, MDA-MB-231) breast epithelial cells were co-cultured with mesenchymal stem cells (MSCs) whereby fusion began in less than 5 min, and up to 2% of the population consisted of hybrid cells after 72 h. In noncancerous tissue, cardiomyocyte-stem cell fusion has been observed, including the transfer of stem cell mitochondria to cardiomyocytes that facilitated cardiomyocyte reprogramming in the context of regenerative medicine. Although cell–cell fusion has been reported in several cancer types, including breast cancer, in vivo mitochondrial exchange via fusion is critically understudied.
Mitochondrial mutations in breast cancer
The metabolic reprogramming of the mitochondrial network of cancer cells is achieved through several mechanisms, including mutations in both nuclear genes encoding mitochondrial proteins and mtDNA.
The mtDNA encodes seven subunits of complex I of the electron transport chain, one subunit of complex III, three subunits of complex IV, and two subunits of complex V. In addition to these polypeptides, mtDNA encodes 22tRNA and 2rRNA. Since mtDNA is not protected by histones, it is more prone to acquiring mutations. Another feature of mtDNA is that approximately 2–10 copies are present per mitochondrion. Further, mutation of each copy may vary from one another. Homoplasmy refers to a state where all copies of mtDNA in a cell share identical sequences. However, once a somatic mutation is introduced, it can propagate either randomly or by positive selection. The latter case results in a heteroplasmic state, which after several rounds of replication can lead to the selection of a dominant clone in the population. As discussed later in this review, such selection can have important consequences on the response of cancer cells to treatment. Because mtDNA encodes for subunits of the electron transport chain, on one hand, mutations in these subunits affect the ability of electrons to be transported efficiently and result in the formation of reactive oxygen species (ROS). ROS, on the other hand, can promote further mutations in mtDNA. Such a vicious cycle supports the notion that mutations in mtDNA may be an early event in tumorigenesis. This has led to an interest in monitoring the number of mtDNA mutations as a prognostic marker of breast cancer.


Overview
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumours. If left unchecked, the tumours can spread throughout the body and become fatal. Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. Cancer cells can spread into nearby breast tissue (invasion). This creates tumours that cause lumps or thickening.

Signs and symptoms
Most people will not experience any symptoms when the cancer is still early hence the importance of early detection. Breast cancer can have combinations of symptoms, especially when it is more advanced. Symptoms of breast cancer can include:
- a breast lump or thickening, often without pain
- change in size, shape or appearance of the breast
- dimpling, redness, pitting or other changes in the skin
- change in nipple appearance or the skin surrounding the nipple (areola)
- abnormal or bloody fluid from the nipple.
People with an abnormal breast lump should seek medical care, even if the lump does not hurt.

As a major energy source for cells, mitochondria are involved in cell growth and proliferation, as well as migration, cell fate decisions, and many other aspects of cellular function. Once thought to be irreparably defective, mitochondrial function in cancer cells has found renewed interest, from suggested potential clinical biomarkers to mitochondria-targeting therapies.
The flow of mitochondria from surrounding cells in breast cancer
Broadly, this phenomenon involves the movement of either whole mitochondria or mtDNA between cells and can be stimulated via several methods, including cell fusion, extracellular vesicles, tunneling nanotubes (TNTs), and through gap junctions (which may be close-ended TNTs). The free release of mitochondria has also been observed in culture medium and human plasma, but it is debated whether they are functional. Cell fusion is the process by which two independent cells partially or fully merge to create a singular cell (permanently or temporarily), thus mixing mitochondria. In vitro, normal (primary cells), neoplastic (MCF10A), and cancerous (MCF7, MDA-MB-231) breast epithelial cells were co-cultured with mesenchymal stem cells (MSCs) whereby fusion began in less than 5 min, and up to 2% of the population consisted of hybrid cells after 72 h. In noncancerous tissue, cardiomyocyte-stem cell fusion has been observed, including the transfer of stem cell mitochondria to cardiomyocytes that facilitated cardiomyocyte reprogramming in the context of regenerative medicine. Although cell–cell fusion has been reported in several cancer types, including breast cancer, in vivo mitochondrial exchange via fusion is critically understudied.

Mitochondrial mutations in breast cancer
The metabolic reprogramming of the mitochondrial network of cancer cells is achieved through several mechanisms, including mutations in both nuclear genes encoding mitochondrial proteins and mtDNA.
The mtDNA encodes seven subunits of complex I of the electron transport chain, one subunit of complex III, three subunits of complex IV, and two subunits of complex V. In addition to these polypeptides, mtDNA encodes 22tRNA and 2rRNA. Since mtDNA is not protected by histones, it is more prone to acquiring mutations. Another feature of mtDNA is that approximately 2–10 copies are present per mitochondrion. Further, mutation of each copy may vary from one another. Homoplasmy refers to a state where all copies of mtDNA in a cell share identical sequences. However, once a somatic mutation is introduced, it can propagate either randomly or by positive selection. The latter case results in a heteroplasmic state, which after several rounds of replication can lead to the selection of a dominant clone in the population. As discussed later in this review, such selection can have important consequences on the response of cancer cells to treatment. Because mtDNA encodes for subunits of the electron transport chain, on one hand, mutations in these subunits affect the ability of electrons to be transported efficiently and result in the formation of reactive oxygen species (ROS). ROS, on the other hand, can promote further mutations in mtDNA. Such a vicious cycle supports the notion that mutations in mtDNA may be an early event in tumorigenesis. This has led to an interest in monitoring the number of mtDNA mutations as a prognostic marker of breast cancer.